Clinic day is a special day, on every mission. It’s the day we get to meet the patients, hear their stories, learn more about their culture and eat more of their food. I have to be honest, we have been spoiled with delicious homemade meals. The local Rotarians and their wives have worked endlessly preparing dishes foreign to most of us. And they never disappoint.
The medical team of surgeons, anesthesiologists, nurses and pediatricians plan out every surgery for the upcoming 10 days of surgeries, and it’s not an easy task. Sometimes, surgery can’t be performed. The patient is either sick, too weak from malnourishment or their families are unable to wait until their scheduled surgery time.
The intake process runs like a well-oiled machine with 6 separate stations all necessary to gather information for a patient’s upcoming surgery.
Step 1: Medical Record: Local volunteers obtain information like their name, address, birthday and reason for the visit. Reynel Nonbrado (left) (pictured here wiuth Quartermaster Mark Syracusa) , both on their first mission, tracks every patient and updates their medical records at the start of the process and throughout the entire mission.

Step 2: Photographer – Numberwoman (myself) on my third mission, and Shultzy (aka Kevin Shultz) on his first, both volunteer Rotarians take photos of each patient.

Step 3: Vitals – Nurses Liz Brown and Tami Schindler, two of our three PACU nurses, take necessary vital signs (temperature, pulse, respiration, blood pressure and oxygen).
 And nurse Ligaya Augustin taking vitals from this young patient.
And nurse Ligaya Augustin taking vitals from this young patient.

Steps 4, 5 and 6 are the most important steps in assessing the patient’s ability to endure a surgical procedure. The patient must be approved at each of these three stations to be included on the surgical schedule.
Step 4: Anesthesia – Dr. Samy Kandasamy (left) and Dr. Tim Conahan (right), seen here with Dr. Brad Coots, assesses every patient to determine how much anesthesia to administer during surgery.

Step 5: Surgeon Assessment: Drs. Matt Schindler and Brad Coots and nurse David Sparks, the medical team, do an evaluation and assessment of a patient to determine what kind of procedure is required.

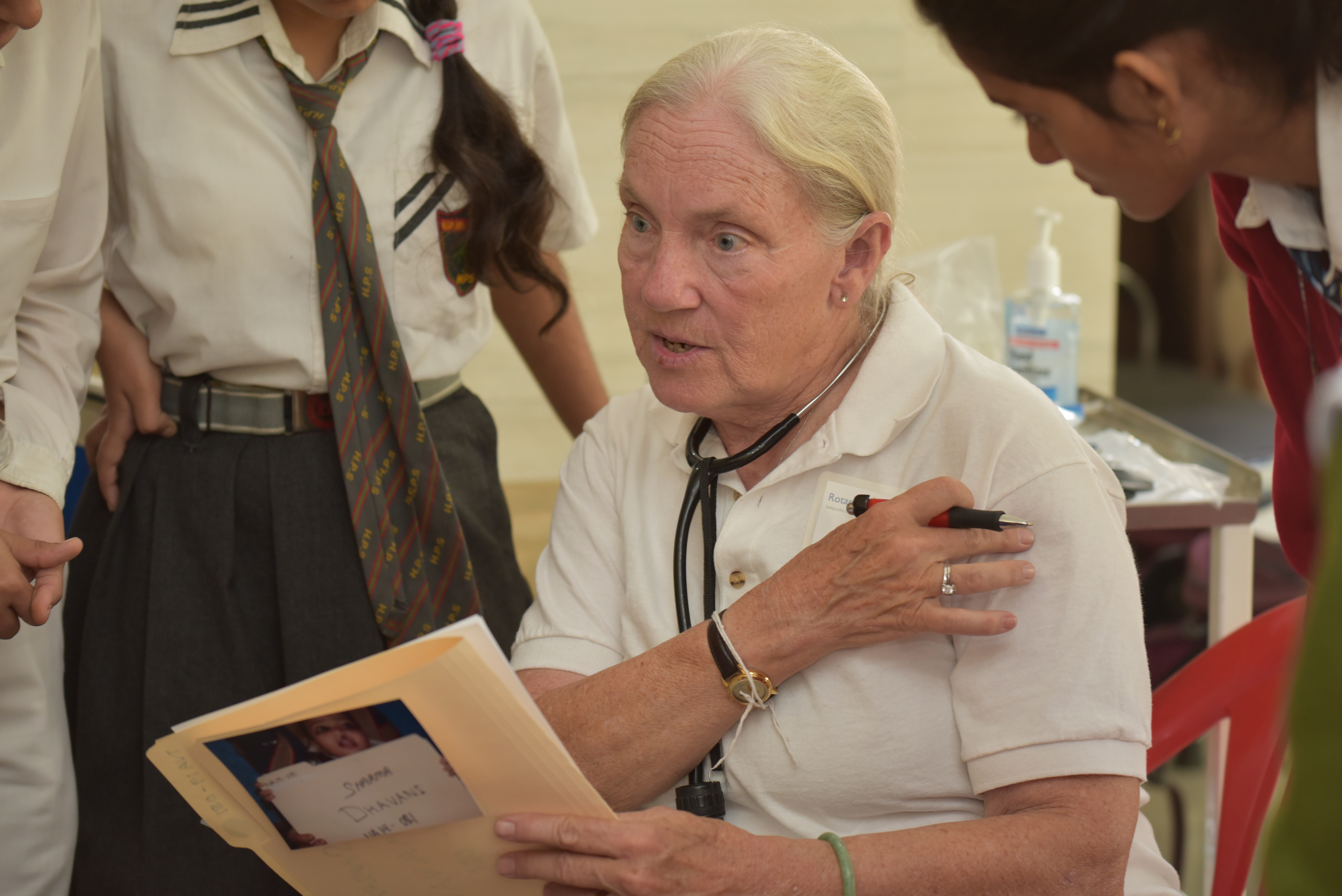
Step 6: Pediatrician – And last but not least, Dr. Barb Rumberger puts it all together. She gathers the patient’s entire medical history, from birth and assesses the overall general health of the patient. Information she gathers of the patient include any prior surgeries, respiratory illnesses and whether they are healthy enough to endure surgery without complications.
The Prequel: The most important step taken starts well before the Rotaplast team starts their mission. Families are ashamed of having a child with a cleft lip and/or palate. The human face is a corridor of emotions, a gateway to verbal and nonverbal communication, and a criterion for social acceptance. Getting past the stigma of having a child with a cleft lip and/or palate and coming to a Rotaplast mission is the biggest step any parent can take!
And these beautiful children are the reasons we are here!